Introduction
Pelvic fractures are serious injuries that can have an enormous impact on a person’s mobility and daily activities. The pelvis is a ring-like bony structure at the base of the spine that connects the trunk to the legs. It plays an elementary role in supporting the body’s weight and protecting internal organs. When the pelvis is fractured, it can lead to severe pain, bleeding, and other complications. This article will explore the causes, types, diagnosis, pelvic fracture treatment options, and its recovery process.

Understanding Pelvic Fractures
A pelvic fracture occurs when one or more of the bones that make up the pelvis are broken. The pelvis consists of several bones, including the ilium, ischium, pubis, sacrum, and coccyx. Pelvic fractures can range from minor cracks in a single bone to severe breaks in multiple bones that destabilise the entire pelvic ring.
There are two main categories of pelvic fractures:
- Stable Fractures: These involve a break in one place in the pelvic ring, with minimal displacement of the bones. The overall structure of the pelvis remains intact.
- Unstable Fractures: These involve two or more breaks in the pelvic ring, causing the bones to become displaced. The pelvis loses its structural integrity.
The severity and stability of a pelvic fracture will determine the appropriate treatment approach and pelvic fracture recovery timeline.
Causes of Pelvic Fractures
Pelvic fractures typically result from high-energy trauma or impacts. Some common causes include:
- Motor vehicle accidents (MVAs) are the most common cause of severe pelvic fractures
- Falls from heights
- Crush injuries
- Pedestrian struck by a vehicle
- Sports injuries (especially in high-impact sports)
- In older adults with weakened bones due to osteoporosis, even minor falls or impacts can cause pelvic fractures. This is known as a fragility fracture.
- Less commonly, repetitive stress on the pelvis from activities like distance running can lead to stress fractures over time.
Diagnosing Pelvic Fractures
Prompt and accurate diagnosis is crucial for pelvic fractures. The diagnostic process typically involves:
Physical Examination:
The doctor will check for pain, bruising, and swelling and assess the stability of the pelvis. They will also evaluate for associated injuries.
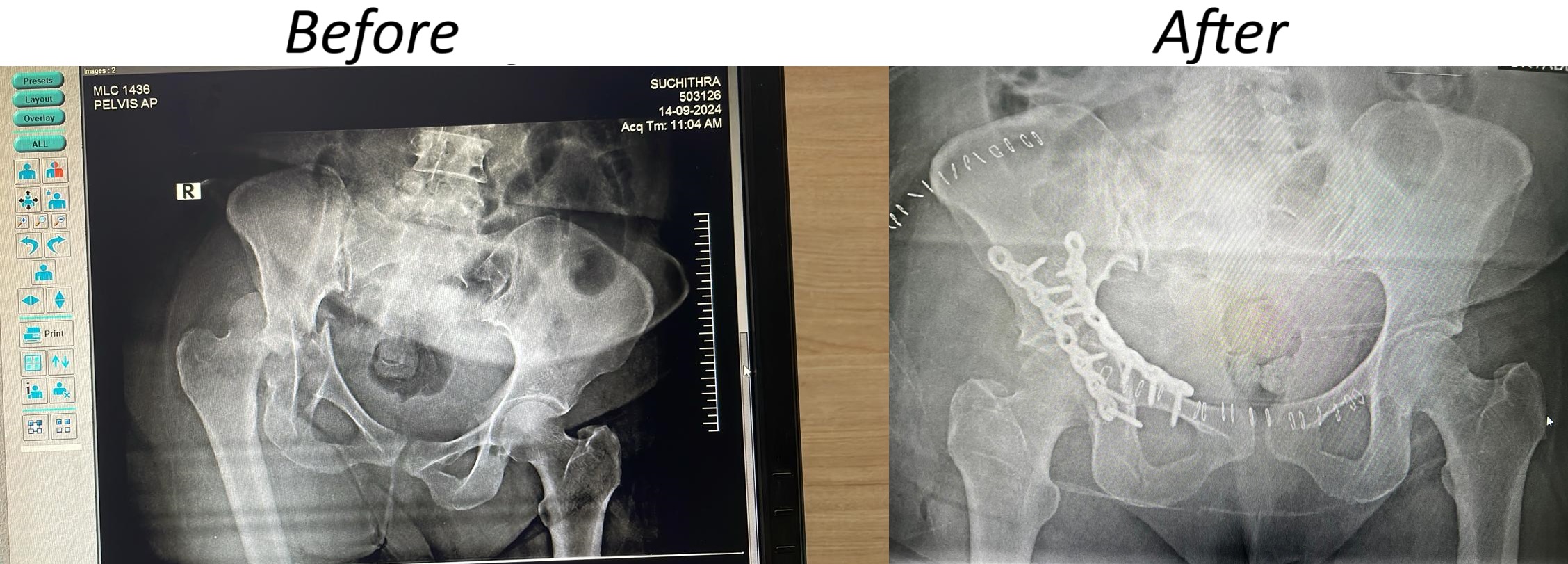
Imaging Tests:
- X-rays: Standard pelvic X-rays are usually the first imaging test performed
- CT Scan: Provides more detailed images to assess fracture patterns and displacement
- MRI: May be used to evaluate soft tissue injuries
Doctors may conduct additional tests like angiography if there are concerns about vascular injuries.
The doctor will use the diagnostic information to classify the type and severity of the pelvic fracture. This guides treatment decisions.
Treatment Options for Pelvic Fractures
Treatment for pelvic fractures depends on the stability of the fracture, associated injuries, and overall health of the patient. Options include:
Non-surgical Treatment:
- For stable fractures with minimal displacement
- It may involve bed rest, pain medication, and gradual mobilisation
- Crutches or a walker are used to avoid weight-bearing on the affected side
- Healing typically takes 8-12 weeks
Surgical Treatment:
- Required for unstable pelvic fractures
- The goals are to realign bones and stabilise the pelvic ring
- External Fixation: Pins or screws inserted into bones and connected to an external frame
- Internal Fixation: Plates and screws used to hold bones in place
For severe pelvic fractures with major bleeding, emergency stabilisation procedures are done first before definitive fracture repair.
Recovery Process for Pelvic Fractures
Broken pelvis recovery is often a long process that requires patience and dedication. The recovery timeline may depend on the severity of the injury but typically involves:
Immediate Post-injury/Post-surgery Phase (1-2 Weeks):
- Pain management
- Preventing complications like blood clots
- Gradual mobilisation as allowed
Early Recovery Phase (2-8 Weeks):
- Increasing mobility with assistive devices
- Physiotherapy to improve strength & range of motion
- Transitioning from bed rest to sitting and standing
Late Recovery Phase (2-6 Months):
- Progressive weight-bearing as the fracture heals
- More intensive physical therapy and exercises
- Regaining independence with daily activities
Long-term Recovery (6-12 Months):
- Return to normal activities and work
- Continued strengthening and conditioning
- Addressing any residual pain or functional limitations
Full recovery can take up to a year or longer for severe pelvic fractures. Patience and compliance with the rehabilitation program are key for optimal outcomes.
Complications and Risks of Pelvic Fractures
While many pelvic fractures heal well with proper treatment, there are potential complications to be aware of:
- Bleeding and Haemorrhage: Pelvic fractures can cause life-threatening internal bleeding
- Nerve Injury: Damage to nerves in the pelvic area can cause pain or numbness
- Urinary/bowel Problems: Injury to organs in the pelvic region
- Blood Clots: Prolonged immobility increases clot risk
- Chronic Pain: Some patients experience ongoing pain even after healing
- Uneven Leg Length: If the fracture heals with deformity
- Post-traumatic Arthritis: Damage to joint surfaces can lead to arthritis
Proper emergency care, surgical techniques, and rehabilitation can help minimise these risks. However, some complications may be unavoidable with severe pelvic trauma.
Conclusion
Pelvic fractures are serious injuries that require prompt diagnosis and appropriate treatment. While recovery can be lengthy, advances in surgical techniques and rehabilitation protocols have improved patient outcomes. With proper care and dedication to the recovery process, most people can regain good function and quality of life after a pelvic fracture. However, severe injuries may still result in long-term limitations or complications.
FAQs
Can I walk around with a broken pelvis?
Walking with a broken pelvis is generally not recommended in the early stages of recovery. Patients may be allowed to walk with crutches or a walker for stable fractures, avoiding weight-bearing on the affected side. For unstable fractures, doctors usually recommend bed rest or wheelchair use initially. The ability to walk depends on the specific fracture pattern and treatment plan.
How long is recovery from a pelvic fracture?
Recovery time varies greatly and depends on the severity of the fracture. Minor, stable fractures may heal in 8-12 weeks. More severe fractures requiring surgery can take 3-6 months for the bones to heal, with full functional recovery taking up to a year or longer. Patients must follow their doctor’s instructions carefully and participate actively in rehabilitation for the best outcomes.
How do you identify a pelvic injury?
Signs and symptoms that may indicate a pelvic injury include:
- Severe pain in the pelvic area, hip, or lower back
- Difficulty or inability to walk or stand
- Numbness or tingling sensation in the groin or legs
- Bleeding from the vagina, rectum, or urethra
- Bruising or swelling in the pelvic region